Here is the prescription for sustainability… In a world where the pharmaceutical industry plays a pivotal role in safeguarding human health, a new, sobering reality has emerged, that the very industry tasked with healing the world is leaving behind an environmental footprint that could endanger it. From antibiotic residues flowing into rivers to emissions from manufacturing hubs in Asia, the pharmaceutical supply chain is facing growing scrutiny. The conversation is no longer just about efficacy and access; it is increasingly about sustainability.
At the heart of this reckoning is the alarming rise of pharmaceutical pollution. This is an issue spotlighted during a landmark virtual workshop hosted by Health Care Without Harm (HCWH) Europe in September 2024. The discussions revealed a stark truth: the industry’s environmental impact spans continents, with Europe heavily dependent on Active Pharmaceutical Ingredients (APIs) and generics manufactured primarily in India and China. The scale is enormous — 70% of all dispensed medications in Europe are generics, and the environmental cost of their production often lies hidden in distant countries.
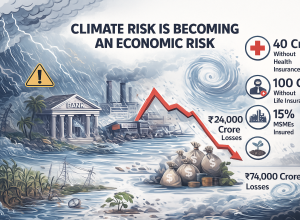
Studies have shown that traces of pharmaceutical compounds, from hormones to antibiotics, are found in over 86% of global river samples, creating unintended side effects on ecosystems and accelerating threats like antibiotic resistance (AMR). With an ageing population, rising chronic illnesses, and the cascading impacts of climate change, pharmaceutical use is projected to skyrocket. In Germany alone, demand is expected to surge by up to 67% by 2045.
The challenge is as complex as it is urgent. Antibiotics, for example, once hailed as miracle drugs, are now contributing to a silent crisis. Their residues often leach into the soil and waterways, disrupting delicate microbial ecosystems and fostering resistant strains of bacteria. Recognizing this, the AMR Industry Alliance, established after the 2016 Davos Declaration, is championing responsible effluent management. It developed a Common Antibiotic Manufacturing Framework, now strengthened with an industry-backed certification scheme via the British Standards Institute. This sets stringent limits on antibiotic emissions from manufacturing plants, ensuring discharges remain below predicted no-effect concentrations.
But global adoption remains uneven. While Nordic countries have begun incorporating environmental standards into their procurement policies, others lag behind. Moreover, the World Health Organization (WHO) has stepped in with even stricter guidelines, including mandatory effluent chemical analysis. Yet, alignment between WHO’s approach and the industry’s remains a work in progress.
Sustainable procurement is emerging as a powerful lever for change. In Europe, where public healthcare accounts for a staggering 40% of GDP, greener purchasing can influence the entire supply chain. HCWH Europe is leading the charge, supporting hospitals and procurement bodies with tools like the Sustainable Procurement Index for Health and guidelines for phasing out chemicals of concern. Governments are beginning to recognize that their purchasing power can either perpetuate pollution or become a force for ecological healing.
Legislation, too, must catch up. The United Nations Environment Programme (UNEP) has pointed out that pharmaceutical pollution is still largely unregulated. The European Green Deal could become a turning point, offering a robust framework to address environmental impacts from “cradle to grave” — from production and packaging to use and disposal. Stronger laws, if implemented with nuance, could drive innovation rather than stifle access, ensuring medicines remain both affordable and environmentally responsible.
Still, legal frameworks alone are not enough. A genuine transformation of the pharmaceutical supply chain requires a paradigm shift. That means moving from treatment to prevention — reducing demand for pharmaceuticals through investments in public health, disease prevention, and lifestyle education. Healthier societies need fewer drugs, lowering both environmental and financial burdens.
Collaboration will be critical. Initiatives like the Pharmaceutical Supply Chain Initiative (PSCI) and Sweden’s PLATINEA platform demonstrate how cross-sector dialogue, involving academia, industry, governments, and civil society, can foster trust and co-create effective solutions. From researchers bridging ecotoxicology gaps to anthropologists tackling social equity, a truly sustainable pharmaceutical future must embrace systems thinking.
Transparency and accountability must also evolve. Public reporting on environmental performance should become standard practice for pharmaceutical firms, guided by global standards like the AMR Alliance’s certification scheme and the upcoming Corporate Sustainability Due Diligence Directive (CSDDD). Yet, careful implementation is vital — too much red tape could choke smaller players and disrupt global medicine access.
Ultimately, greening the pharmaceutical supply chain is not just a technical challenge, it is a moral imperative. At stake is not just the integrity of ecosystems or the purity of rivers, but the very health of the communities these medicines are meant to serve. The solutions lie in innovation, legislation, collaboration, and above all, a shared recognition that healthcare must do no harm, not only to people but to the planet we all depend on.